The prevalence of tobacco smoking declined in all regions for males between 1990 and 2019, with the fastest rate of decline observed in the Latin America and Caribbean region and the slowest in the North Africa and Middle East region.
The fastest rate of decline in females was observed in the Latin America and the Caribbean region followed by the South Asia region. Prevalence of tobacco smoking for females increased in the Central Europe, Eastern Europe, and Central Asia region in the first decade of the 21st century but declined thereafter (Figure 13a and Figure 13b).
For males, age-standardized smoking prevalence was almost 50% in the Southeast Asia, East Asia, and Oceania region, with the next highest levels in the Central Europe, Eastern Europe, and Central Asia region (39.5%), and the lowest observed in the SubSaharan Africa region (17.5%) and Latin America and Caribbean region (17.1%).
For females, age-standardized smoking prevalence was highest in the High-Income region (17.6%) and Central Europe, Eastern Europe, and Central Asia region (15.5%) and lowest in the Sub-Saharan Africa region (2.9%).
For males, the five countries with highest prevalence were Timor-Leste (64.6%), Kiribati (63.8%), Federated States of Micronesia (62.2%), Indonesia (58.3%) and Armenia (55.3%) . The five with the lowest prevalence were Peru (7.3%), Nigeria (7.4%), Sao Tome and Principe (7.8%), United States Virgin Islands (8.3%) and Guinea Bissau (8.5%).
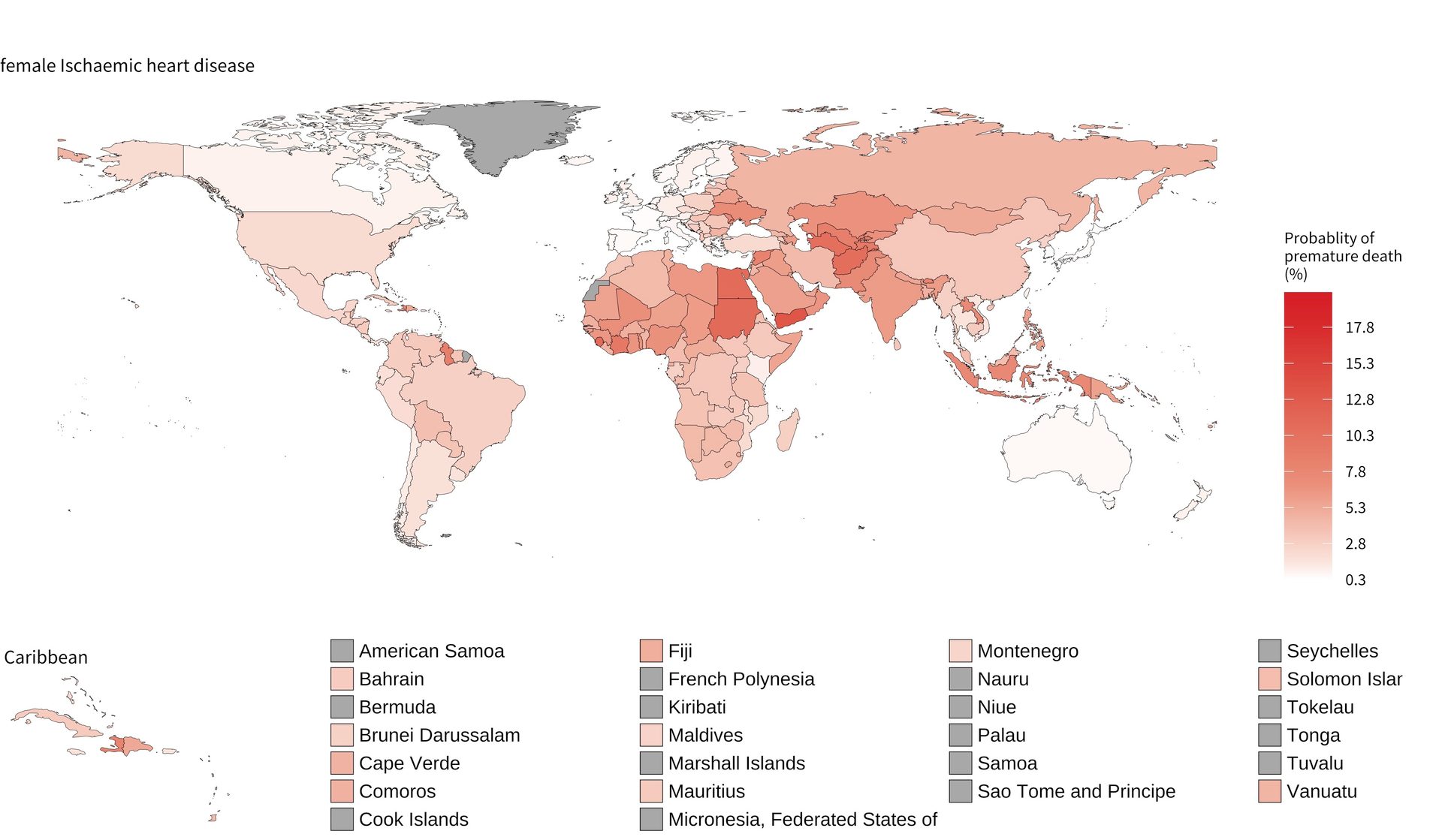
For females, the five countries with the highest prevalence were Greenland (42.3%), Nauru (40.3%), Serbia (37.8%), Federated States of Micronesia (36.4%) and Kiribati (35.1%). ).
Those with the lowest prevalence were Eritrea (0.7%), Egypt (1.1%), Morocco (1.1%), Guinea Bissau (1.1%) and Nigeria (1.2%).
In all countries except Sweden and Ireland, the agestandardised prevalence of tobacco smoking was higher in males than females.